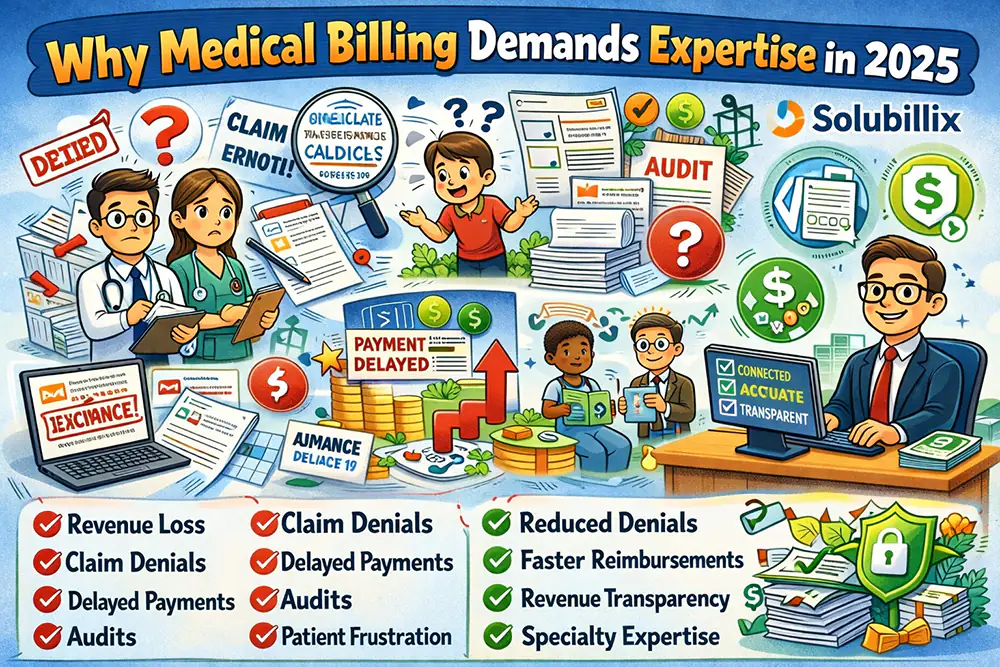
Healthcare billing is no longer just about submitting claims. It is a complex, compliance-driven, payer-specific ecosystem where even minor errors can lead to revenue loss, denials, delayed payments, audits, and patient dissatisfaction. From evolving CPT/ICD-10 updates to payer-specific policies, value-based care, and patient responsibility growth, providers need a medical billing company that delivers accuracy, transparency, and measurable financial results.
Solubillix stands out as a results-driven medical billing company built to maximize reimbursements, reduce denials, and give providers full control of their revenue cycle.
What Is Solubillix?
Solubillix is a full-service medical billing and revenue cycle management (RCM) company designed to support healthcare providers across multiple specialties. Our mission is simple:
Increase collections, reduce administrative burden, and ensure compliant, timely reimbursement.
We combine industry expertise, payer intelligence, advanced workflows, and hands-on account management to deliver consistent financial performance for medical practices of all sizes.
Why Solubillix Is the Most Trusted Medical Billing Company
1. End-to-End Revenue Cycle Management
Solubillix manages the entire revenue cycle, ensuring no revenue leakage at any stage:
- Patient demographics & insurance verification
- Eligibility & benefits validation
- Accurate medical coding (CPT, ICD-10, HCPCS)
- Claim creation and electronic submission
- Denial prevention & denial management
- Appeals and follow-ups
- Payment posting & reconciliation
- Patient billing & credit balance resolution
- A/R cleanup and aging reduction
This holistic approach ensures that claims are correct before submission, not fixed after denial.
2. Specialty-Focused Billing Expertise
Unlike generic billing companies, Solubillix provides specialty-specific billing workflows. Our team understands the nuances of documentation, modifiers, payer rules, and medical necessity requirements.
We support (but are not limited to):
- Primary Care & Family Medicine
- Behavioral Health & Psychiatry
- OB/GYN & Women’s Health
- Internal Medicine
- Urgent Care
- Mental Health & Therapy Services
- Multi-specialty Group Practices
Each specialty has unique denial risks—Solubillix builds safeguards into the billing process to protect revenue.
3. Advanced Denial Management & Appeals
Denials are one of the largest causes of lost revenue. Solubillix implements proactive and reactive denial strategies:
- Root-cause analysis by denial category
- Payer-specific appeal templates
- COB and eligibility dispute resolution
- Medical necessity & documentation-based appeals
- Timely filing and reconsideration tracking
Our denial specialists work aggressively to recover revenue that other billing companies write off.
4. Clean Claim Strategy = Faster Payments
At Solubillix, we follow a Clean Claim First-Pass Acceptance methodology:
- Real-time claim scrubbing
- Modifier validation
- NCCI and LCD/NCD checks
- Provider credentialing verification
- Payer rule compliance
This results in:
- Higher first-pass acceptance rates
- Faster reimbursements
- Lower rework costs
- Reduced A/R days
5. Transparent Reporting & Financial Visibility
Providers deserve clarity—not confusion. Solubillix delivers easy-to-understand, actionable reporting, including:
- Monthly collection performance
- Aging A/R reports (30/60/90/120+)
- Denial trend analysis
- Payer performance insights
- Patient responsibility tracking
- Credit balance reports
Our reporting empowers providers to make informed financial and operational decisions.
Compliance, Accuracy & Security
Solubillix operates with strict compliance standards:
- HIPAA-compliant workflows
- Secure data handling protocols
- Regular internal audits
- Up-to-date coding and payer rule training
We protect both provider revenue and patient trust.
Patient-Friendly Billing Experience
A strong revenue cycle also improves patient satisfaction. Solubillix supports:
- Clear, easy-to-understand patient statements
- Accurate patient responsibility calculations
- Payment posting transparency
- Credit balance management
- Reduced billing disputes
This leads to fewer complaints, better collections, and stronger patient relationships.
Why Solubillix Outperforms Other Medical Billing Companies
| Feature | Solubillix | Traditional Billing Companies |
| Specialty Expertise | ✔ Yes | ❌ Limited |
| Denial Recovery Focus | ✔ Aggressive | ❌ Reactive |
| Transparent Reporting | ✔ Detailed & Clear | ❌ Basic |
| Compliance-Driven | ✔ Yes | ❌ Inconsistent |
| Dedicated Account Support | ✔ Yes | ❌ Shared Teams |
SEO Keywords Naturally Targeted in This Content
- Medical billing company
- Revenue cycle management services
- Medical billing services
- Healthcare billing solutions
- Denial management services
- Insurance billing experts
- HIPAA-compliant billing company
- RCM company for providers
This content is optimized for high-intent healthcare searches while remaining natural and authoritative.
Final Thoughts: The Solubillix Advantage
Choosing the right medical billing company directly impacts a provider’s financial health. Solubillix is more than a billing vendor—we are a revenue partner committed to accuracy, accountability, and long-term growth.
If you are looking for:
- Higher collections
- Fewer denials
- Faster payments
- Complete revenue transparency
Solubillix is the medical billing company you can trust.
Ready to Optimize Your Revenue Cycle
Partner with Solubillix and experience billing done right—accurate, compliant, and results-driven.
Why Payers Are Flagging More Claims Than Ever
Introduction: A Record Surge in Flagged & Suspended Claims
Healthcare providers across the U.S. are experiencing an unprecedented increase in flagged, pended, and manually reviewed insurance claims. Even practices with historically strong clean-claim rates are seeing more requests for documentation, delayed payments, and unexplained rejections.
This is not accidental.
Payers have fundamentally changed how claims are evaluated. Advanced analytics, AI-driven fraud detection, stricter medical necessity enforcement, and aggressive cost-containment strategies have created a claims environment where every detail matters more than ever before.
This guide explains why payers are flagging more claims, what triggers payer scrutiny, and how providers can protect revenue in this new billing reality.
Benchmarking Against National & Regional Utilization Data
Payers now benchmark every provider against:
- National utilization averages
- Specialty-specific billing norms
- Geographic peer comparisons
If a provider bills above average—even legitimately—claims are more likely to be flagged.
Examples include:
- Higher-than-average E/M levels
- Frequent add-on codes
- Increased telehealth utilization
- Higher therapy or behavioral health visit frequency
This approach allows payers to preemptively flag claims before overpayment occurs.
Modifier Overuse Is Triggering Automated Flags
Modifiers are essential— they are also one of the fastest ways to trigger payer audits.
High-risk modifiers include:
- Modifier 25 (significant, separately identifiable E/M)
- Modifier 59 (distinct procedural service)
- Telehealth modifiers (95, GT)
- Modifier 24 and 57
When modifiers appear frequently without bulletproof documentation, claims are flagged—even if historically paid.
Increased Focus on Fraud, Waste & Abuse (FWA)
Federal and commercial payers are under pressure to reduce healthcare spending. As a result, FWA monitoring has expanded dramatically.
Payers now flag claims for:
- Upcoding patterns
- Unbundling indicators
- Excessive visit frequency
- Duplicate or overlapping services
- Time-based billing inconsistencies
⚠️ Important: A flagged claim does not mean fraud—but repeated flags increase audit risk.
Documentation Quality Is Being Actively Scored
In 2025, documentation quality itself is evaluated.
AI tools analyze:
- Note completeness
- Clinical progression between visits
- Time documentation accuracy
- Use of cloned or repetitive language
Poor-quality documentation—even with correct codes—raises red flags and increases claim scrutiny.
Coordination of Benefits (COB) Errors Are Under Heavy Surveillance
COB-related issues have become a major focus area.
Claims are frequently flagged for:
- Conflicting primary vs secondary coverage
- Inaccurate subscriber information
- Employer group changes not reflected
- Medicare coordination mismatches
Even minor COB discrepancies can cause automatic claim suspension.
Telehealth & Behavioral Health Claims Face Extra Scrutiny
Telehealth expansion has permanently changed payer policies.
In 2025, telehealth and behavioral health claims are flagged for:
- Location and POS mismatches
- Modality inconsistencies (audio vs video)
- State licensing verification
- Frequency and duration validation
- Documentation alignment with telehealth rules
These services remain high-risk categories for payer review.
Payers Are Delaying Payments Strategically
Not all flagged claims are denied.
Some are intentionally delayed through:
- Additional documentation requests
- Repeated reconsideration cycles
- Manual review queues
This strategy improves payer cash flow while testing provider follow-up strength.
How Providers Can Reduce Claim Flagging
To survive and thrive in this environment, providers must adapt.
Best Practices:
- Strengthen diagnosis specificity
- Align CPT codes tightly with documentation
- Audit modifier usage regularly
- Monitor utilization benchmarks
- Improve documentation quality—not length
- Track denial and flag trends by payer
- Use specialty-focused billing expertise
📈 Practices that implement proactive billing controls experience faster payments and fewer denials.
Final Thoughts: Billing Accuracy Is No Longer Optional
In 2025, payer scrutiny is not temporary—it is the new standard.
Claims are flagged not only for errors, but for patterns, trends, and perceived risk. Providers who rely on outdated billing processes will continue to face delayed payments and rising denials.
Success now depends on precision, documentation integrity, payer intelligence, and proactive revenue cycle management.
About Solubillix
Solubillix helps providers navigate this complex billing environment with payer-aware billing strategies, denial prevention workflows, and compliance-driven RCM solutions.
If your claims are being flagged more frequently, the problem may not be your care—it may be your billing strategy.
Solubillix turns payer scrutiny into predictable revenue.
Medical Billing Errors That Cost Providers Thousands Each Year
Introduction: The Silent Revenue Drain in Medical Practices
Medical billing errors are one of the largest hidden causes of revenue loss for healthcare providers. Unlike denied claims that are clearly visible, many billing mistakes quietly reduce reimbursement, delay payments, or cause underpayments that are never recovered.
Industry data and payer behavior trends show that even small, repeatable billing errors can cost providers tens of thousands of dollars per year—especially for practices with high claim volume.
This guide breaks down the most common medical billing errors, why they happen, how they impact revenue, and what providers can do to prevent them and beyond.
1. Inaccurate or Incomplete Patient Demographics
One of the most basic—and costly—billing errors starts at the front desk.
Common Issues:
- Misspelled patient names
- Incorrect date of birth
- Wrong insurance ID numbers
- Missing subscriber information
- Outdated employer or plan details
Revenue Impact:
Claims with demographic errors are often rejected immediately, delaying payment and increasing rework costs.
📉 Even a 1–2% demographic error rate can significantly increase denial volume.
2. Eligibility & Benefits Verification Failures
Many claims are billed without proper eligibility confirmation.
Frequent Mistakes:
- Billing inactive insurance
- Missing authorization requirements
- Ignoring benefit limitations
- Incorrect primary vs secondary insurance
Revenue Impact:
- Denials for no coverage
- Increased patient balances
- Write-offs that could have been avoided
Eligibility errors shift financial responsibility from payer to provider.
3. Incorrect or Outdated Medical Coding
Coding errors remain one of the top reasons for claim denials and underpayments.
Examples:
- Using outdated CPT or ICD-10 codes
- Insufficient diagnosis specificity
- Incorrect code sequencing
- Failure to follow payer-specific coding rules
Revenue Impact:
- Downcoded claims
- Partial payments
- Increased audit risk
Accurate coding is no longer optional—it is a revenue protection strategy.
4. Modifier Misuse or Overuse
Modifiers are powerful—but risky.
High-Risk Modifiers:
- Modifier 25
- Modifier 59
- Telehealth modifiers (95, GT)
- Modifier 24 and 57
Common Errors:
- Applying modifiers without documentation support
- Overusing modifiers across visits
- Copying modifier patterns from prior claims
Revenue Impact:
Modifiers trigger automated payer scrutiny, increasing denials and audit exposure.
5. Weak or Incomplete Documentation
Documentation quality directly impacts reimbursement.
Red Flags for Payers:
- Generic or cloned notes
- Missing medical necessity justification
- Poor linkage between diagnosis and procedure
- Inaccurate time-based documentation
Revenue Impact:
Even correctly coded claims can be denied if documentation does not fully support the service.
6. Failure to Track and Appeal Denials
Many practices do not aggressively manage denied claims.
Common Problems:
- Missing appeal deadlines
- No root-cause denial analysis
- Writing off recoverable claims
Revenue Impact:
Denied claims that are not appealed result in permanent revenue loss.
📌 A large percentage of denied claims are recoverable when appealed correctly.
7. Untimely Filing Errors
Each payer has strict filing deadlines.
Causes:
- Delayed charge entry
- Incorrect payer submission
- Clearinghouse issues not followed up
Revenue Impact:
Untimely filing denials are often non-recoverable, resulting in full write-offs.
8. Poor Payment Posting & Reconciliation
Payment posting errors hide underpayments.
Examples:
- Not comparing EOBs to contracted rates
- Missing secondary insurance payments
- Incorrect patient responsibility posting
Revenue Impact:
Underpayments go unnoticed, costing providers revenue they are contractually owed.
9. Ignoring A/R Aging Trends
Aging accounts receivable is a warning signal.
Common Issues:
- Excessive balances over 90 or 120 days
- No payer-specific follow-up strategy
- Lack of accountability
Revenue Impact:
Older A/R becomes harder to collect and increases write-offs.
10. Lack of Revenue Cycle Oversight
Without consistent monitoring, billing errors compound.
Signs of Poor Oversight:
- No regular billing audits
- No KPI tracking
- Limited payer performance analysis
Revenue Impact:
Small inefficiencies multiply into major financial losses.
How Providers Can Prevent Costly Medical Billing Errors
Best Practices:
- Verify eligibility before every visit
- Improve documentation quality
- Use payer-specific coding rules
- Audit modifier usage
- Track denials by root cause
- Monitor A/R aging weekly
- Reconcile payments accurately
Final Thoughts: Accuracy Equals Revenue
Medical billing errors are not just administrative issues—they are financial threats.
In today’s payer environment, precision, compliance, and proactive billing management are essential. Practices that identify and fix billing errors early protect revenue, improve cash flow, and reduce stress across their organization.
About Solubillix
Solubillix helps healthcare providers eliminate costly billing errors through specialty-focused coding, denial prevention strategies, and end-to-end revenue cycle management.
If billing errors are costing your practice money, the solution is not more work—it’s smarter billing.
Solubillix turns accuracy into revenue.