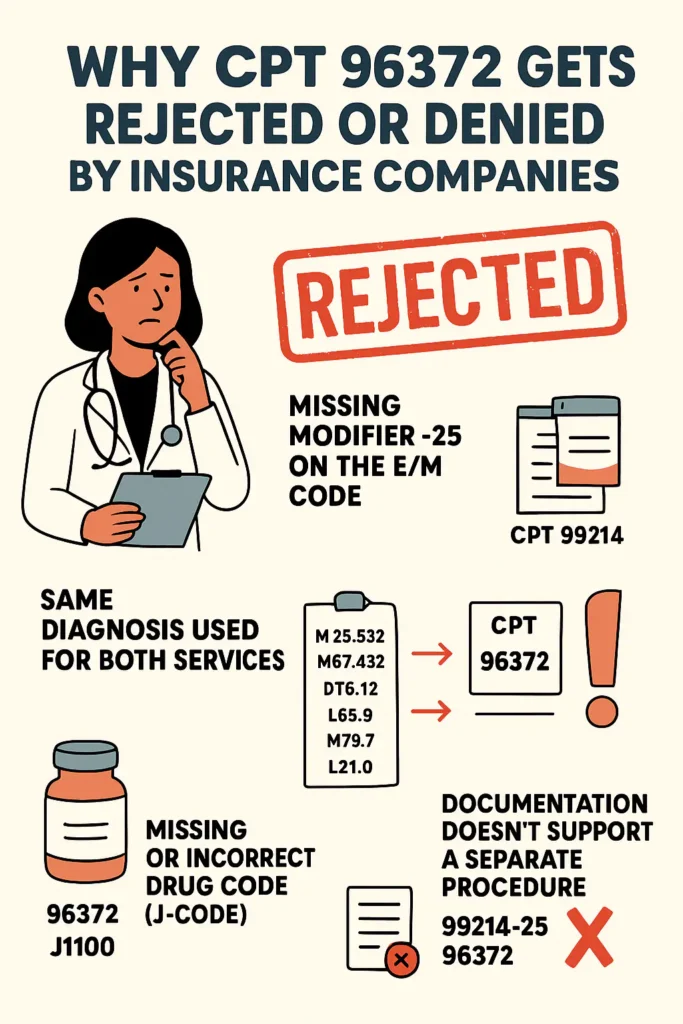
In medical billing, one of the most common claim rejections practices encounter is related to CPT 96372 – Therapeutic, Prophylactic, or Diagnostic Injection (specify substance or drug; subcutaneous or intramuscular).
Even though it’s a routine procedure in urgent care, family medicine, and specialty practices, incorrect claim setup often leads to payer denials or SmartEdit rejections. Understanding why 96372 gets denied helps your team protect revenue and maintain compliance.
⚠️ 1. Missing Modifier –25 on the Evaluation and Management Code
When CPT 96372 is billed with an E/M service (99213, 99214, etc.) on the same date, most payers automatically bundle the injection into the visit unless modifier –25 is appended to the E/M code.
Why it happens:
The payer system assumes the injection was part of the same evaluation and not a distinct procedure.
Compliance Fix:
Add modifier –25 to the E/M code when documentation supports a separately identifiable service.
✅ Example: 99214-25 and 96372
🧾 2. Same Diagnosis Used for Both Services
Using the same diagnosis code for 99214 and 96372 often triggers an “unbundling” rejection.
If both lines show the same ICD-10, payers see it as duplicate work under one condition.
Compliance Fix:
Assign a separate diagnosis for the injection procedure whenever appropriate.
Example:
- 99214-25 → J06.9 (Upper respiratory infection)
- 96372 → M79.1 (Myalgia – Toradol injection)
🩹 3. Missing or Incorrect Drug Code (J-Code)
CPT 96372 represents only the administration. The drug itself must also be billed using the correct HCPCS J-code (e.g., J1100 for Dexamethasone, J0696 for Ceftriaxone).
Compliance Fix:
Always pair the injection admin code with the proper J-code and accurate units.
Example: 96372 (×1) + J1100 (×2)
🧠 4. Documentation Doesn’t Support a Separate Procedure
Insurance reviewers look for clear, distinct notes supporting both the E/M and the injection.
If the clinical note doesn’t mention the injection rationale, drug, dosage, and site, the payer may deny it as “not medically necessary” or “included in E/M service.”
Compliance Fix:
Include in your documentation:
- Drug name and strength
- Route and site of administration
- Medical necessity for the injection
- Provider signature and date/time
💻 5. Billing Software or Setup Errors
Sometimes, denials are caused by incorrect claim configuration:
- Missing facility taxonomy
- Expired CLIA number
- Wrong billing location (e.g., rendering provider NPI used as billing provider)
Compliance Fix:
Check your practice management system settings for accurate billing NPI, taxonomy, and CLIA details before resubmitting.
🔢 6. NCCI (National Correct Coding Initiative) Edits
Under NCCI, CPT 96372 is bundled with several codes unless modifier –25 (E/M) or –59 (procedure-to-procedure) is justified.
Payers such as UnitedHealthcare, BCBS, and Medicare use these edits to prevent duplicate payment for related services.
Compliance Fix:
Review the current NCCI edit table before submitting claims, or use claim scrubbers that automatically alert you of conflicts.
💬 7. Payer-Specific Policy Restrictions
Some payers, including Medicaid programs, may have additional restrictions:
- Limited number of injection reimbursements per visit
- Specific diagnosis or prior authorization requirements
- Coverage limited to in-office administration
Compliance Fix:
Review each payer’s medical and billing policy for CPT 96372 to ensure compliance before claim submission.
💡 How to Prevent Future 96372 Denials
- Use –25 modifier whenever billing 96372 with E/M codes.
- Ensure separate diagnosis for injection when medically justified.
- Include drug J-code and NDC when required.
- Verify documentation and payer policy before claim submission.
- Keep taxonomy and CLIA information current in your billing system.
- Perform periodic claim audits to detect recurring errors early.
🤝 How SoluBillix Helps Providers
At SoluBillix, we specialize in compliance-based claim scrubbing and revenue recovery. Our billing experts:
- Identify CCI edit conflicts before submission,
- Verify modifiers and diagnosis linkage,
- Ensure complete documentation for injections, and
- Reduce denials through payer-specific billing protocols.
With SoluBillix as your billing partner, you can focus on patient care while we safeguard your revenue cycle accuracy.