When it comes to medical billing, claim accuracy is essential for smooth revenue recovery. One denial code many practices struggle with is CO-151, which often relates to service frequency or repeat billing. This guide breaks down everything providers need to know—causes, compliance requirements, resolution steps, and how Solubillix helps reduce denials through automation and intelligent billing workflows.
What Is Denial Reason Code CO-151?
CO-151 — “Payment adjusted because the payer deems the information submitted does not support this many/frequency of services.”
This denial indicates that the payer believes:
- The service was billed too frequently
- The visit exceeds plan-allowed limits
- A repeat procedure wasn’t properly justified
- Documentation does not support multiple units/visits
It is a frequency-based or repeat-service compliance denial.
Primary Causes of CO-151 Denials
Understanding why this denial occurs helps providers prevent significant revenue loss.
1. Exceeding Insurer Frequency Limits
Certain CPT/HCPCS codes have payer-defined limits such as:
- Once per day
- Once per 12 months
- Limited number of therapy sessions per year
- Annual screening caps
If billing doesn’t align with these rules, CO-151 is triggered.
2. Duplicate or Repeat Services
Submitting:
- The same CPT on the same DOS
- Same NPI and patient
- No correct repeat modifier (76/77)
can cause automated rejection by payer claims editors.
3. Missing or Insufficient Documentation
If chart notes do not support:
- Medical necessity
- Repeat testing
- Multiple units billed
- Time requirements (for therapy codes)
the payer may decline the claim.
4. Incorrect Coding or Unit Billing
Common coding errors:
- Billing incorrect units
- Missing primary code for add-on CPTs
- Unbundled services without appropriate modifiers
- Accidentally copying forward previous encounters
5. Plan Benefit Limitations
The patient may have:
- Reached maximum allowable visits
- Exceeded policy benefit limits
- No coverage for repeat service
- Restrictions on diagnostic services
How to Fix a CO-151 Denial?
Below is a structured, compliance-friendly workflow for resolving this denial.
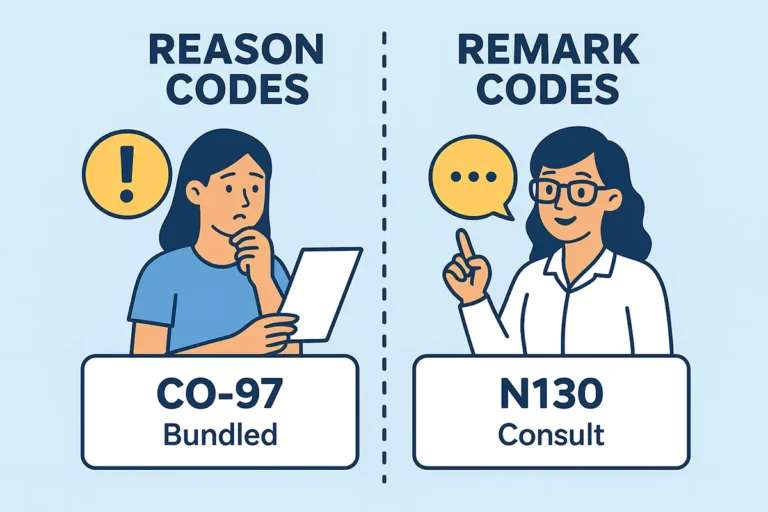
Step 1: Review the EOB/ERA for Remark Codes
Look for any related notes such as:
- M97 – Service exceeds frequency guidelines
- N130 – Consult payer’s policy
- MA130 – Authorization missing
These help clarify the exact frequency rule you violated.
Step 2: Verify the Patient’s Benefits
Confirm:
- Allowed visit limits
- Annual maximums
- Time-frame between repeat procedures
- Whether previous claims have already consumed benefits
Step 3: Examine Provider Documentation
Ensure the records contain:
- History of condition
- Medical necessity for repeated services
- Progress notes for each visit
- Procedure details supporting units or repeat billing
Step 4: Correct the Claim Before Resubmission
This may include:
- Adding modifier 76 (repeat procedure by same provider)
- 77 (repeat procedure by different provider)
- 59/X modifiers for distinct services
- Fixing unit errors
- Rebilling with accurate CPT combinations
Step 5: Submit a Clear and Well-Documented Appeal
If the denial is incorrect:
- Attach detailed chart notes
- Include provider justification
- Provide payer-specific policy references
- Request reconsideration
How to Prevent CO-151 Denials: Compliance Best Practices
1. Real-Time Eligibility and Frequency Checks
Before providing a service, verify:
- Annual benefit limits
- Repeated service restrictions
- Coverage time intervals
2. Accurate Modifier Usage
Use repeat-service modifiers correctly:
- 76 – Repeat procedure by same provider
- 77 – Repeat procedure by another provider
- 59/XE/XU – Distinct service when allowed
3. Maintain Thorough Clinical Documentation
Documentation should clearly capture:
- Reason for repeat visit
- Clinical progression
- Results of previous tests
- Treatment plan justification
How Solubillix Helps Reduce CO-151 Denials
Solubillix offers smart, automated, and compliance-focused billing technology designed to minimize denial trends—including CO-151. With built-in payer logic and intelligent workflow features, Solubillix ensures your claims are accurate before submission.
Below are the ways Solubillix strengthens your RCM performance:
✨ Denial Analytics & Root-Cause Tracking
Solubillix shows:
- Which CPTs commonly get CO-151
- Payer-specific patterns
- Provider-based error trends
- Denial recurrence timelines
This empowers your team to fix the underlying causes—not just each denial.
Conclusion
CO-151 is a frequency-based denial that often results from missing modifiers, repeated submissions, insufficient documentation, or benefit limitations. By adopting proper verification, documentation, coding, and compliance workflows, providers can significantly reduce these denials.
With Solubillix, practices benefit from:
- Real-time eligibility
- Smart documentation audits
- Denial analytics
This leads to clean claims, faster reimbursements, and fewer CO-151 denials.