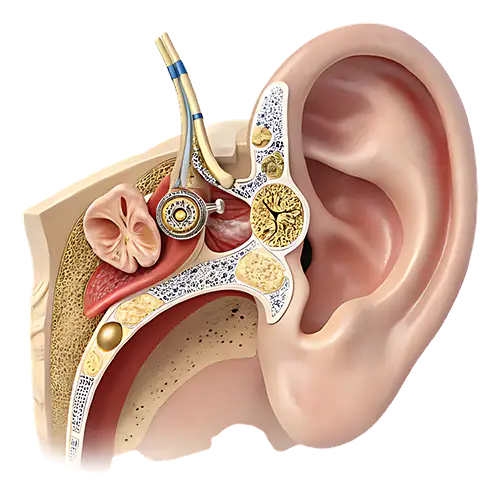
Optical Coherence Tomography (OCT) of the ear is a diagnostic imaging procedure that allows providers to view detailed structures of the middle ear. While clinically useful, these services are reported with Category III CPT codes, which means they are considered emerging technology and are often scrutinized by payers.
The relevant codes include:
- 0458T – This code represents an OCT imaging study of the middle ear when it is performed on one side (unilateral), and the results are submitted without a full written interpretation.
- 0486T – This code is used when OCT imaging of the middle ear is performed on both sides (bilateral), and the provider also prepares and submits an interpretation/report of the findings.
Code Level and Why It Matters
Both 0458T and 0486T are Category III codes.
- Category III codes are temporary CPT codes used for emerging technologies, services, and procedures.
- They do not yet have widespread clinical acceptance, FDA approval in some cases, or sufficient peer-reviewed evidence to support their general medical necessity.
- As a result, many insurance payers automatically flag or deny these services as “experimental” or “investigational.”
Because of their Category III status, payers often require extensive medical documentation and may not offer standard reimbursement.
Why Insurance Denies OCT of the Ear
Denials for CPT 0458T and 0486T usually occur for the following reasons:
- Investigational/Experimental Classification
- Most carriers classify these codes as investigational due to insufficient long-term studies and lack of inclusion in national coverage guidelines.
- No Established Medical Necessity
- Payers frequently deny claims when documentation does not clearly demonstrate why OCT was clinically required for diagnosis or treatment planning.
- Incorrect Code Usage
- Some billers mistakenly use ophthalmic OCT codes (e.g., 92132) instead of the correct ear-related codes, triggering denials.
- Lack of Pre-Authorization
- Because these codes are not widely covered, prior authorization is often required. Submitting without it leads to automatic denial.
- Modifier and Laterality Errors
- Improper use of RT, LT, or 50 modifiers causes compliance issues since Category III codes have specific instructions for unilateral and bilateral reporting.
Common Billing Mistakes Other Billers Make
Unfortunately, many billing teams run into denials with 0458T and 0486T. The most frequent compliance and billing errors include:
- Incorrect Code Selection
- Billers sometimes confuse OCT of the ear (0458T/0486T) with ophthalmic OCT (e.g., 92132), leading to denials for “not medically necessary” or “incorrect procedure.”
- This confusion happens because both codes reference OCT technology but apply to entirely different anatomical sites.
- Missing or Insufficient Documentation
- Payers require clear documentation showing why the test was performed, the clinical findings, and a proper interpretation/report for 0486T.
- Submitting claims without the provider’s interpretation or without linking to a diagnosis code supporting medical necessity often results in rejection.
- Improper Modifier Usage
- Some billers fail to apply the correct modifiers when the service is performed unilaterally vs. bilaterally.
- Others incorrectly append modifiers like -RT, -LT, or -50, causing conflicts with Category III coding guidelines.
- Lack of Prior Authorization or Payer Verification
- Since these are relatively new and specialized procedures, not all insurance plans cover them. Billers sometimes skip pre-checking coverage, leading to outright denials.
- Non-Compliance with Category III Code Rules
- Category III codes are often considered “experimental or investigational.” Submitting them without a compliance-based approach (medical policy review, payer coverage confirmation, and documentation alignment) increases denial rates.
How Solubillix Handles OCT of the Ear Billing Professionally
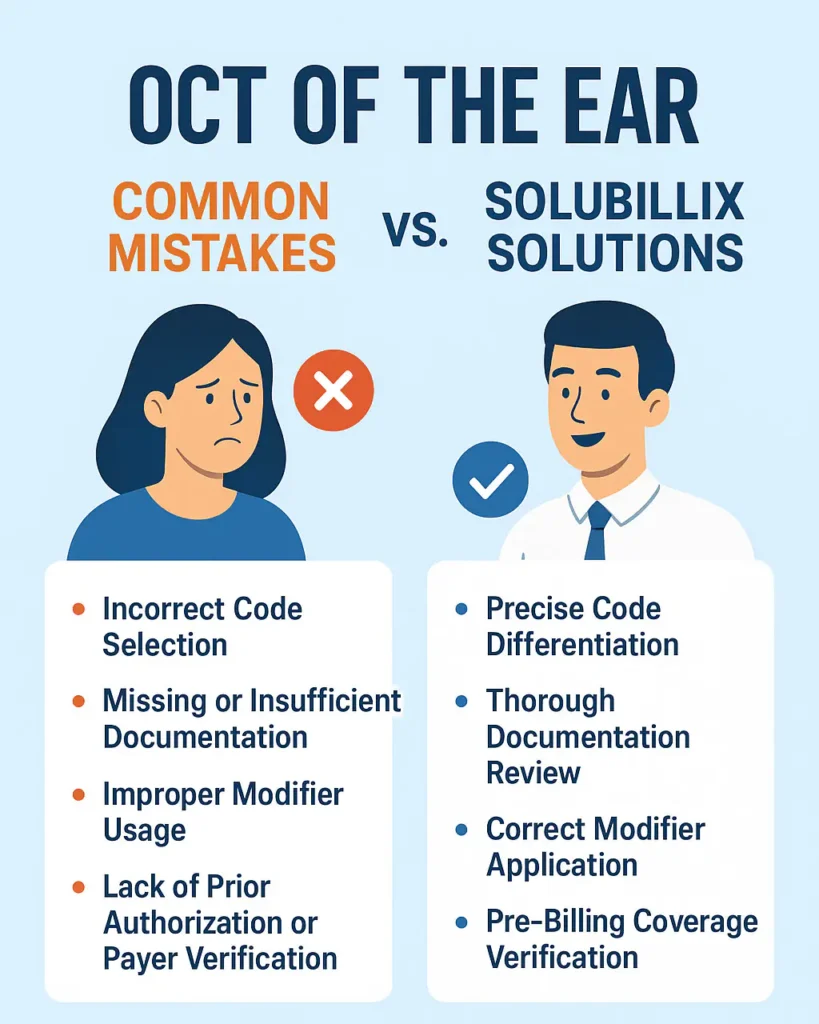
At Solubillix, we take a compliance-driven approach to ensure accurate claim submission and maximum reimbursement for OCT procedures:
- Precise Code Differentiation
- Our team is trained to distinguish OCT of the ear from ophthalmic OCT and other imaging codes, eliminating cross-coding errors.
- Thorough Documentation Review
- We verify that every claim includes the physician’s interpretation, detailed medical notes, and correct ICD-10 codes that justify the test.
- Correct Modifier Application
- We apply RT/LT modifiers only when appropriate and avoid misuse of bilateral modifiers, aligning with CPT and payer-specific rules.
- Pre-Billing Coverage Verification
- Before submitting claims, we confirm payer policies and prior authorization requirements for 0458T and 0486T, reducing unnecessary denials.
- Compliance Monitoring
- Our billing process is anchored in audit-ready compliance, meaning every OCT claim is submitted with full documentation and aligned with payer medical necessity guidelines.
✅ Conclusion
Billing for OCT of the ear (0458T and 0486T) requires an expert approach because these codes are Category III and often denied as investigational. Many billers make mistakes by misapplying codes, skipping policy checks, or failing to provide adequate documentation.
Solubillix brings compliance, accuracy, and payer-specific expertise to ensure providers reduce denials and capture every possible reimbursement opportunity.