Payers are organizations or entities responsible for financing or reimbursing the cost of healthcare services. These can include insurance companies, government programs, or other organizations that offer financial coverage for medical care. Their primary role is to process claims submitted by healthcare providers and determine the reimbursement amount for the services rendered.
Types of Payers
Payers can be categorized into several types based on their structure and funding sources:
Government Payers
These are public healthcare programs funded by federal and state governments to provide medical coverage for specific populations. Medicare covers individuals aged 65 and older, as well as younger people with disabilities. Medicaid offers health coverage to low-income individuals and families, while the Children’s Health Insurance Program (CHIP) provides insurance for children in families whose incomes are too high for Medicaid but too low for private insurance.
Commercial Payers
Private insurance companies, such as UnitedHealthcare, Aetna, and Cigna, fall into this category. They offer a range of health plans to individuals and groups, often negotiating rates with healthcare providers. Plans vary based on employer group needs or individual preferences.
Private Payers
This category includes non-insurance payment methods like direct cash payments from patients or financing arrangements. It can also refer to specialized insurance plans provided by smaller companies or organizations outside of large commercial insurers.
Self-Pay Patients
Some patients opt to pay for their medical services out-of-pocket without involving an insurance provider. These self-pay arrangements may involve negotiated rates directly between the patient and the healthcare provider.
Functions of Payers in Medical Billing
Payers perform several essential functions within the medical billing process:
1. Claim Processing
After a healthcare provider submits a reimbursement claim, the payer reviews and processes it. This includes verifying patient information, checking coverage eligibility, and determining if the services rendered qualify for reimbursement.
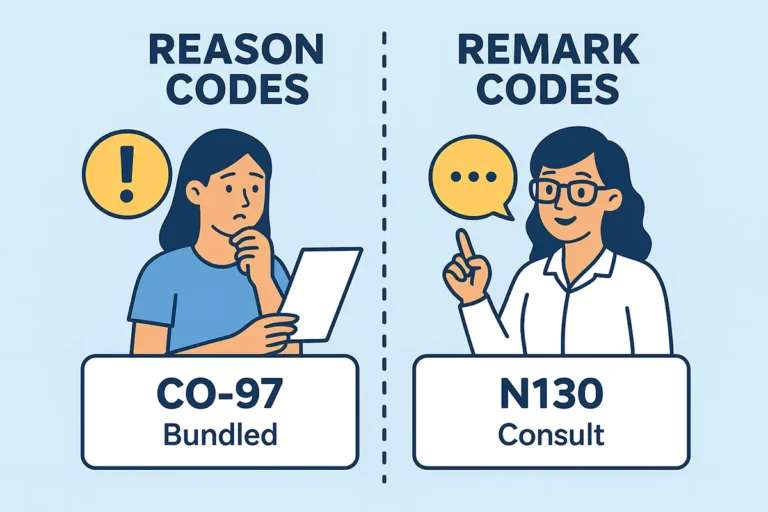
2. Claim Adjudication
The payer evaluates claims based on factors such as medical necessity, the patient’s coverage plan, and contractual agreements with providers. During this process, claims can be approved, denied, or adjusted in accordance with the payer’s policies.
3. Payment Issuance
Once a claim is approved, the payer issues payment to the healthcare provider following the agreed contract terms. The reimbursement may only cover part of the billed amount, factoring in deductibles, co-pays, and co-insurance responsibilities.
4. Network Management
Payers manage networks of contracted healthcare providers to control costs and ensure quality care. They negotiate rates with these providers while ensuring patients have access to necessary services within the network.
5. Customer Support
Payers offer customer service to assist both patients and providers with questions about coverage, claim status, and billing disputes. This support is vital for resolving reimbursement-related issues and ensuring smooth communication.
Importance of Payers in Healthcare Service
Payers play a vital role in maintaining the financial stability of healthcare systems by providing necessary funding for medical services. Their importance can be summarized as follows:
- Financial Support: Payers contribute to covering the costs of medical treatments and services, enabling patients to receive necessary care without shouldering the full financial burden.
- Cost Control: Through rate negotiations with providers and effective network management, payers help regulate healthcare expenses while ensuring the delivery of high-quality care.
- Data Analytics: Payers gather extensive data on patient care and treatment outcomes, which can be analyzed to identify healthcare trends and enhance care delivery strategies.
- Quality Improvement: Many payers are shifting toward value-based care models that emphasize quality over quantity. This approach fosters collaboration between payers and providers to achieve better patient outcomes.