In medical billing, the National Provider Identifier (NPI) is one of the most critical elements for claim submission. It identifies the healthcare provider or facility delivering the service, and payers use it to process claims, apply network rules, and determine reimbursement.
When it comes to urgent care centers versus primary care practices, both use NPIs, but there are key differences in how they are issued, how they are classified, and how billing is handled.
What Is an NPI?
An NPI (National Provider Identifier) is a unique 10-digit number assigned by the Centers for Medicare & Medicaid Services (CMS) to healthcare providers and organizations.
- Type 1 NPI – Assigned to individual providers (e.g., physicians, nurse practitioners).
- Type 2 NPI – Assigned to organizations or facilities (e.g., clinics, urgent care centers, hospitals).
Urgent Care NPI vs. Primary Care NPI
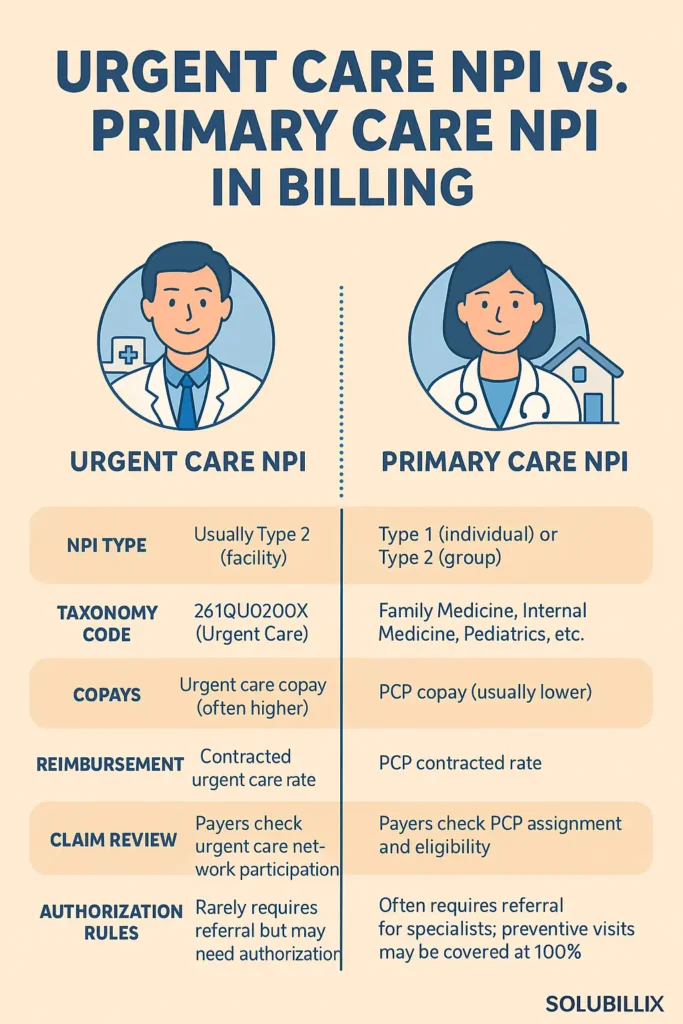
1. Urgent Care NPI
- Typically, a Type 2 (organizational) NPI, registered as an urgent care facility.
- Identified under the taxonomy code 261QU0200X (Clinic/Center – Urgent Care).
- Used when the practice is licensed, credentialed, and recognized by payers as an urgent care provider.
- Claims billed under an urgent care NPI are processed differently than primary care, often subject to:
- Urgent care copays (separate from PCP or specialist copays).
- Different reimbursement rates based on payer contracts.
- Specific payer network requirements for urgent care services.
2. Primary Care NPI
- May be a Type 1 NPI (individual provider such as a family physician or internist) or a Type 2 NPI (primary care group practice).
- Uses taxonomy codes like 207Q00000X (Family Medicine) or 207R00000X (Internal Medicine).
- Claims are recognized as primary care visits and typically:
- Apply primary care copays (often lower than urgent care copays).
- Follow preventive care and chronic care billing rules.
- May require patient assignment to a PCP under HMO or Medicare Advantage plans.
Key Billing Differences
| Aspect | Urgent Care NPI | Primary Care NPI |
| NPI Type | Usually Type 2 (facility) | Type 1 (individual) or Type 2 (group) |
| Taxonomy Code | 261QU0200X (Urgent Care) | Family Medicine, Internal Medicine, Pediatrics, etc. |
| Copays | Urgent care copay (often higher) | PCP copay (usually lower) |
| Reimbursement | Contracted urgent care rate | PCP contracted rate |
| Claim Review | Payers check urgent care network participation | Payers check PCP assignment and eligibility |
| Authorization Rules | Rarely requires referral but may need authorization depending on payer | Often requires referral for specialists; preventive visits may be covered at 100% |
| Denial Risks | If billed under the wrong taxonomy or NPI, claim may be denied as “not urgent care” | If billed under urgent care codes with PCP NPI, claim may process incorrectly |
Compliance Considerations
- Credentialing: Providers must ensure that their NPIs are properly registered with the correct taxonomy (urgent care vs. primary care).
- Contracting: Insurance payers contract urgent care centers differently than primary care practices, which impacts reimbursement.
- Billing Accuracy: Using the wrong NPI or taxonomy can cause denials, underpayments, or incorrect patient responsibility (wrong copay applied).
- Audit Risks: Misrepresentation of urgent care vs. primary care services can raise compliance concerns if claims are not aligned with the registered NPI.
How Solubillix Ensures Compliance
At Solubillix, we help providers avoid these costly errors by:
- Verifying NPI type and taxonomy before claim submission.
- Aligning billing with payer contracts to ensure correct reimbursement.
- Preventing denials caused by NPI mismatches or incorrect classification.
- Educating staff on when to bill under urgent care vs. primary care to reduce compliance risk.
✅ Conclusion
The difference between an urgent care NPI and a primary care NPI lies in taxonomy, payer recognition, reimbursement structure, and patient responsibility. Billing under the wrong NPI can result in denials, incorrect copays, or compliance issues. By ensuring NPIs are properly classified and claims are billed accurately, providers can maximize reimbursement and remain compliant with payer requirements.