Running a behavioral health practice is a balancing act. On one hand, you’re providing compassionate care, helping people through some of their most vulnerable moments. On the other hand, you’re running a business that depends on accurate billing and consistent reimbursement to survive.
For many providers, it’s the business side that becomes overwhelming. Insurance rules, coding requirements, prior authorizations, compliance updates—it feels like a never-ending maze. And unfortunately, even small slip-ups in billing can cost practice thousands of dollars in lost revenue every year.
At Solubillix, we understand this struggle. That’s why we’ve positioned ourselves not just as a billing service, but as your billing partner. We take an active role in helping providers avoid common mistakes, clean up problem areas, and build a revenue cycle that supports growth instead of draining energy.
Let’s talk honestly about where behavioral health providers often trip up—and how we help fix it.
The Documentation Dilemma
The Challenge:
Therapists and counselors pour their hearts into patient care. But when it comes to charting and documentation, it’s easy to miss details like start and stop times, treatment objectives, or progress updates. To an insurance company, missing details can make the difference between a paid claim and a denial.
How We Help:
At Solubillix, we review your documentation with an expert eye before claims ever go out. We share feedback, provide user-friendly templates, and make sure your notes check all the boxes insurers are looking for. This keeps claims clean, denials low, and reimbursements timely—without putting more burden on you.
Coding Confusion
The Challenge:
Behavioral health codes can be tricky. They change often, and they vary depending on the payer. A small error—like using the wrong code for an intake versus a therapy session—can lead to rejected claims or underpayments.
How We Help:
Our certified coders specialize in behavioral health. We stay up-to-date with every CPT change and payer guideline, so you don’t have to. We also run regular coding audits to catch small issues before they turn into big problems. That means your claims are accurate, compliant, and optimized for maximum reimbursement.
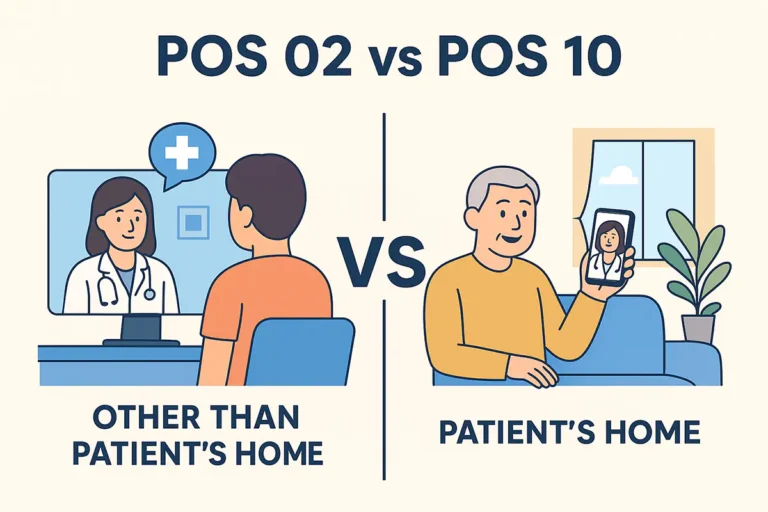
Insurance Surprises
The Challenge:
Imagine seeing a new patient, providing great care, and then discovering their insurance doesn’t cover the service. Now you’re stuck either writing off the session or sending an unexpected bill to the patient. Both scenarios hurt your bottom line and your relationship with the client.
How We Help:
Solubillix verifies benefits and eligibility before the session happens. We confirm coverage for telehealth, check visit limits, and identify co-pays and deductibles. We then give you and your patients clear information up front, so everyone knows what to expect—no financial surprises, no awkward conversations.
The Prior Authorization Trap
The Challenge:
Some services require prior authorization. If you skip that step, the claim gets denied, no matter how perfectly it’s coded.
How We Help:
We take prior authorizations off your plate. Our team submits requests, follows up with payers, and keeps track of renewals so nothing slips through the cracks. That means you never lose revenue simply because paperwork wasn’t filed in time.
Keeping Up with Compliance
The Challenge:
Insurance rules and government regulations are constantly evolving. Providers who don’t stay updated can end up out of compliance—or worse, flagged for an audit.
How We Help:
At Solubillix, staying on top of compliance changes is part of our daily routine. We keep track of new payer policies, coding updates, and industry regulations, then adjust your billing practices accordingly. You don’t have to worry about chasing updates—we’ve already handled them.
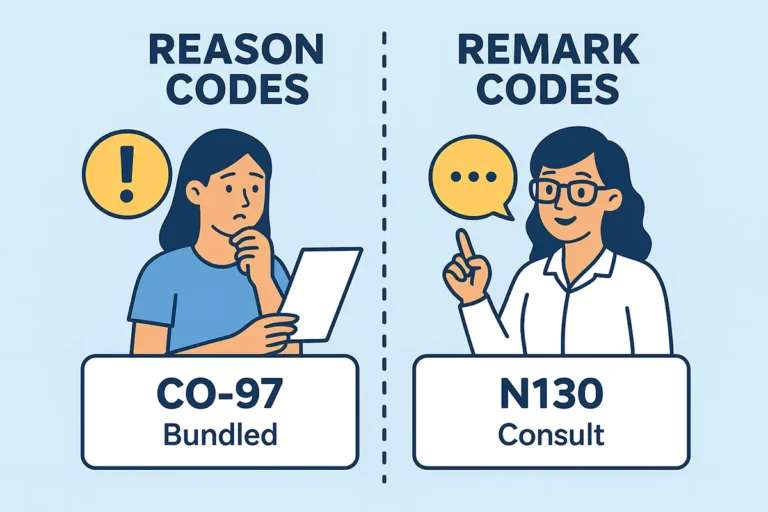
Denials That Slip Away
The Challenge:
Submitting a claim is just the first step. Denials and underpayments require follow-up, appeals, and persistence. Many practices simply don’t have the time to chase every issue, which means money is left on the table.
How We Help:
We don’t stop at claim submission. At Solubillix, we track every claim until it’s resolved. If something gets denied, we jump on it—appealing, resubmitting, and fighting for the payment you deserve. We also provide detailed reporting so you can see exactly where revenue is being lost and recovered.
Why Providers Choose Solubillix
The providers we work with tell us the same thing: billing used to feel like a constant battle, but now it feels like a system they can rely on. That’s because we don’t just process claims—we partner with you to protect your revenue and give you peace of mind.
When you choose Solubillix, you’re choosing:
- A team that understands behavioral health inside and out.
- Accurate, efficient billing that reduces denials.
- Proactive compliance and coding support.
- Full transparency into your revenue cycle.
- More time for you to focus on patient care, not paperwork.
Final Word
Behavioral health providers do some of the most important work in healthcare, but the financial side shouldn’t get in the way of that mission. At Solubillix, our job is to keep your billing smooth, accurate, and profitable so you can keep your focus exactly where it belongs—on your patients.
Slip-ups will always exist in healthcare billing. But with your billing partner Solubillix by your side, they don’t have to cost you revenue, time, or peace of mind. Together, we’ll make sure your practice is financially healthy, so you can continue helping others stay mentally healthy.