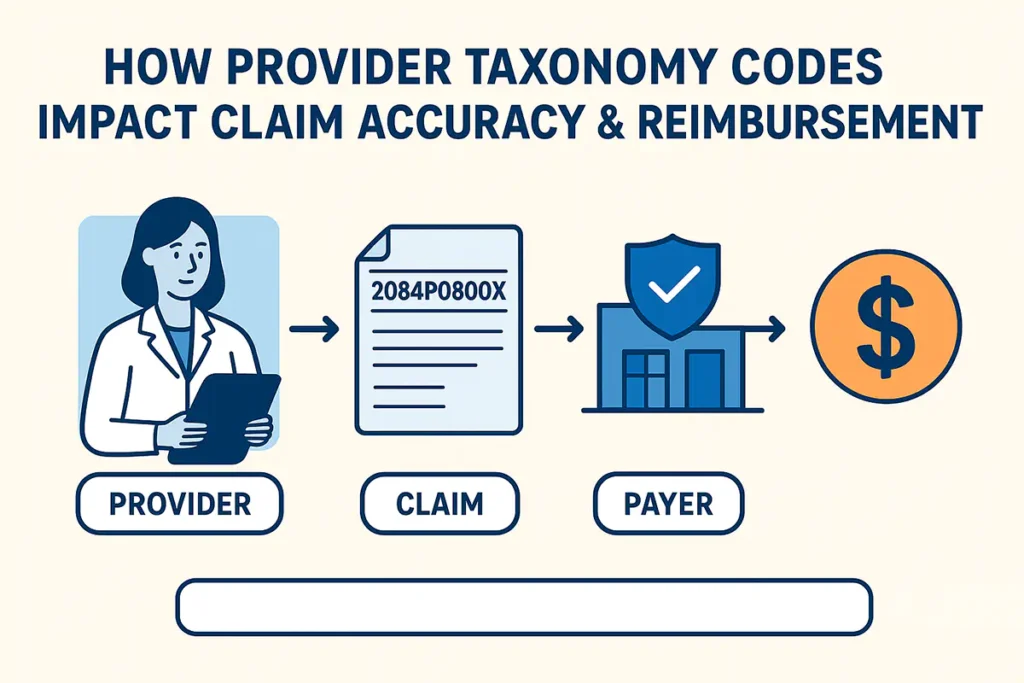
In the healthcare billing environment, even the smallest coding error can delay payment or lead to claim denials. Among those often-overlooked details, Provider Taxonomy Codes play a crucial role in ensuring claims are routed, verified, and paid accurately.
For providers and billing professionals, understanding the proper use of taxonomy codes is not only about getting paid — it’s about maintaining billing integrity, payer compliance, and proper provider credentialing. At Solubillix, we help practices manage these requirements seamlessly so providers can stay compliant and focus on quality patient care.
💡 What Are Provider Taxonomy Codes?
A Provider Taxonomy Code is a unique, 10-character alphanumeric identifier that classifies healthcare providers by their specialty, subspecialty, and service type. These codes are maintained by the National Uniform Claim Committee (NUCC) and are essential in multiple stages of the billing and credentialing process.
They are used to:
- Identify the provider’s specialty on insurance claims
- Match provider type with their National Provider Identifier (NPI)
- Support accurate payer enrollment and credentialing
- Facilitate proper claim routing and reimbursement
Each provider must use the taxonomy code that most accurately reflects their practice specialty.
For example:
- Clinical Social Worker — 1041C0700X
- Psychiatric Nurse Practitioner — 363LP0808X
- Behavioral Health & Psychiatry — 2084P0800X
- Primary Care/Internal Medicine — 207R00000X
Choosing an incorrect taxonomy code or mismatching it with a provider’s NPI can lead to claim denials, rejections, or even compliance reviews by payers.
⚖️ Why Provider Taxonomy Codes Matter for Reimbursement
Taxonomy codes are the bridge between provider identity and claim recognition. When the code on a claim doesn’t align with the provider’s enrollment or NPI record, payers may question the provider’s eligibility to perform or bill for that service.
Common Reimbursement Issues Linked to Incorrect Taxonomy Codes
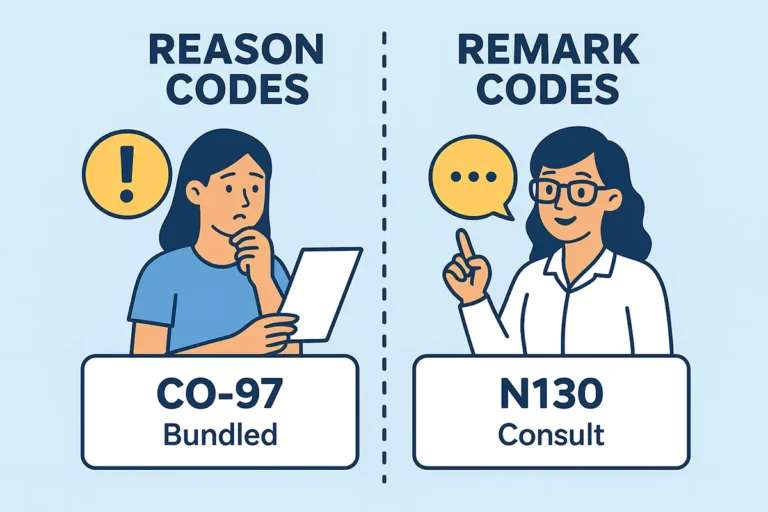
- Claim Rejections Due to Mismatch:
If the taxonomy code submitted on the claim does not match the code registered in the NPI database or with the payer, the claim may be automatically rejected. - “Provider Not Eligible to Bill” Denials:
Payers often deny claims when the taxonomy code does not correspond with the billed CPT or HCPCS code. For example, if a claim for psychotherapy is billed under an internal medicine taxonomy, it will not process correctly. - Credentialing and Enrollment Conflicts:
When credentialing departments use one taxonomy code and the billing department uses another, payers may not properly recognize the provider, leading to processing delays or enrollment errors. - Audit Risk:
Repeated taxonomy discrepancies may raise red flags with auditors or compliance teams, increasing the risk of post-payment reviews or recoupments.
These issues directly affect reimbursement turnaround times and can disrupt revenue flow — especially for high-volume behavioral health or multi-specialty practices.
🧾 Compliance Requirements Around Taxonomy Codes
Regulatory bodies and payers require taxonomy codes to be accurate, consistent, and traceable. Compliance is tied to the following key regulations and standards:
- HIPAA Transactions and Code Sets Rule:
Requires taxonomy codes to be included in all electronic claims (ANSI X12 837 format) for provider identification. - CMS (Centers for Medicare & Medicaid Services):
Uses taxonomy codes to validate provider eligibility for specific claim types and to determine reimbursement under Medicare rules. - REMS and Specialty Program Requirements:
For certain behavioral health or specialty services (e.g., Spravato, TMS), payers may require taxonomy validation to confirm the provider’s specialty aligns with approved billing categories.
To maintain compliance, every provider record — including NPI registration, CAQH profile, and payer credentialing file — must use the same taxonomy information.
💼 How Solubillix Helps Providers Stay Accurate and Compliant
At Solubillix, we understand how much administrative burden inaccurate provider data can create. Our billing and compliance team proactively manages taxonomy-related requirements to ensure claims are submitted correctly the first time.
Here’s how we help:
✅ 1. Taxonomy Verification and Alignment
We review and verify each provider’s taxonomy code against the NPI Registry, CAQH, and payer credentialing data to confirm consistency before claim submission.
✅ 2. Credentialing and Enrollment Support
Our credentialing experts ensure that every taxonomy code used during enrollment matches the billing data — reducing mismatched claims and credentialing delays.
✅ 3. Smart Claim Scrubbing
Our billing system automatically checks that each claim includes the correct taxonomy code and matches the corresponding CPT or HCPCS code based on payer-specific rules.
✅ 4. Compliance-Driven Documentation
Solubillix maintains documentation standards aligned with HIPAA, CMS, and payer guidelines, ensuring all provider classifications are properly recorded and traceable in the event of an audit.
✅ 5. Training and Ongoing Support
We educate billing staff and provider teams on the importance of taxonomy coding accuracy, keeping them informed about updates in NUCC listings or payer policy revisions.
🚀 The Solubillix Advantage
Provider taxonomy management may seem like a small part of the billing process, but it directly influences claim acceptance rates, compliance, and revenue integrity.
By partnering with Solubillix, providers gain a trusted ally that ensures every code, claim, and credentialing record is fully aligned with payer and regulatory standards.
Our mission is simple —
to protect your practice from compliance risks, reduce denials, and help you get reimbursed faster, accurately, and compliantly.